QUALITY ASSURANCE OF PERSONAL PROTECTIVE APPAREL AT TERTIARY HOSPITALS IN YOLA, ADAMAWA STATE
Main Article Content
Abstract
Background: Exposure to ionizing radiations is hazardous to radiological workers, patient’s relatives and patients. The effect may be stochastic or deterministic. Protective apparel keeps the radiation dose received by hospital workers, patients and patient relatives as low as reasonable achievable (ALARA) under normal working conditions. Protective apparels are frequently mishandled in the diagnostic room after use leading to damage.
Objective: This study aimed at assessing integrity of the protective apparel used at the radiology department of a tertiary health institution in Adamawa State of Nigeria.
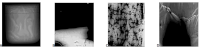
Methods: From three different hospitals in Yola, 26 pieces of protective apparels were identified, inspected and classified by the hospital, type, manufacturer's name, years it had been used, and the thickness of the lead. With 17 x 14-inch cassette two exposures
were made on each the garment with 70 kVp and 10 mAs with a film focal distance (FFD) of 100cm with a conventional x-ray unit..
Results: The result showed 12 (46.0 %) of the protective apparel studied were defective with split 5 (42.0%), crack 4(33.0%) and hole 3(25.0%) as the most common defect. Correlation of the apparels age and the number of defective protective apparels were statistically not significant (p = 0.166).
Conclusion: In order ensure protective garments provide the best protection possible; there is a need for proper storage and regular quality assurance on the apparels in the radiology departments to ensure radiation protection.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
All articles in JRRS are published under the Creative Commons Attribution 4.0 International License (CC BY 4.0). This permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
How to Cite
References
1. Do, K-H. General Principles of Radiation Protection in Fields of Diagnostic Medical Exposure. J Korean Med Sci 2016;31: S6-9
http://dx.doi.org/10.3346/jkms.2016.31.S1.S6
2. Alhassan, M. Khan, B. Baraya, Jt. Evaluation of 1.5mm Lead Shield for Radiological Protection and Comparison of Calculated and Measured Results of Equivalent Dose. J. Appl. Sci. Environ. Manage. 2019; 23(12) 2195-2199 DOI: https://dx.doi.org/10.4314/jasem.v23i12.17
3. Oyar O. Kislaliglu A. How protective are the lead aprons we use against ionizing radiation? Diagn Interve Radiol [journal]
2012;18(2):147–152. DOI: 10.4261/1305-3825.DIR.4526-11.1 ·
4. Stam, W. and Pillay, M. Inspection of lead aprons: A Practical Rejection Model. The Rad Safety J. [e-journal] 2008;95(2) 133136.Available at http://www.infabcorp.com/ downloads/leadapron-inspection.pdf. [Accessed 14/8/ 2021].
5. Bjorka, W.L. Blo, S. Rekdal, M.K. Rusandu, A. Quality of radiation protection aprons and quality control routines at different diagnostic imaging modalities. Radiography Open [ejournal ] 2020;6 1-10 available at https://journals.oslomet.no/index.php/radopen/
index [accessed on 15/8/2021]
6. Michel, R. Michael J. Z. Implementation of an X-ray Radiation Protective Equipment - Inspection Program Health Phys. 2002;82
(Supp1ementl):S51453
7. Livingstone RS, Varghese A. A simple quality control tool for assessing integrity of lead equivalent aprons. Indian J Radiol Imaging.
2018;28(2) 258-62. DOI: 10.4103/ijri.IJRI_374_1
8. Finnerty M,, Brennan PC. Protective aprons in imaging departments: Manufacturer stated lead equivalence values require validation. Eur Radiol 2005;15:1477-84.
9. Omojola, A.D. Akpochafor, M.O. Adeneye, S.O. Aniekop, U.P. Radiographic assessment of protective aprons and dose simulation to
personnel. J of Radiation and Cancer Research. 2019;10(2). 117-23. DOI: 10.4103/jrcr.jrcr_14_19
10. Franken, Y. Huyskens, CJ. Guidance on the use of protective lead aprons in medical radiology Protection efficiency and correction
factors for personal dosimetry. Centre for Radiation Protection, Eindhoven University of Technology. The Netherlands 2002. available @ https://www.researchgate.net/publication/ [accessed on 21/8/2021]
11. University of Iowa Hospital and clinics, policy and procedure manual, diagnostic servicesradiology intergrity of lead aprons and thyroid shield DS-R-05.55. 2017 available at www.medicine.uiowa.edu [accessed on 15/8/2021]
12. Lambert K, McKeon T. Inspection of lead aprons: Criteria for rejection. Health Phys. 2001; 80. S67- 69
13. Nkubli BF, Nzotta CC, Nwobi IC, Moi SA, Luntsi G, Salisu U, Matthew A. Quality control in radiology units of tertiary healthcare centers in North Eastern Nigeria. NJMIRT.2013; 2:26-31.
14. Anas, M. Nzotta. C.C., Nkubli BF. Abubakar, U. Bappah, SY. Osayaba, PE. Dukku AA. A survey of diagnostic X-ray Room design and
shielding integrity of lead aprons in a state in north eastern Nigeria. J Radigr Radiat sci. 2020;34: 42-50
15. Chiegwu, HU. Ugwuanyi, DC. Okeji, MC. Onwugalu, E. How Efficient Are The Lead Aprons Used For Radiation Protection In Our
Hospitals? 2018;8(2) 52-55 ISSN - 2249-555x
16. Ukpong E.V., Eduwem D.U., Efanga I. EsienUmo E. James N.A An Assessment of the Lead rubber aprons in Radiodiagnostic centres in
South-South Nigeria. . J Radigr Radiat sci., 2010;24:1 – 7
17. Daniel, O.A. Xaviera IC. integrity test of lead apron and its effect on personnel and carers Bangabandhu sheik Mujib Med univ. J
2018;11: 34-37 available @ www.banglajol.info [accessed on 10/8/2021]
18. Oppliger-Schäfer D, Roser HW. . Quality Assurance of X-Ray Protection Clothing at the University Hospital Basel Radiological
Physics, University Hospital Basel Basel. 2009;1–5 available at https://ssrpm.ch/old/2009/10 [accessed on 15/8/2021]
19. Duran, E. B. and Phillips, B. Rejection criteria for defects in lead apparel used for Radiation protection of x-ray workers. BC Centre for
Disease Control 2003.
20. Bawazeer, O. Quality Assurance of Personal Radiation Shield for Kilovoltage Photon: A Multicentre Experience. Dove Press journal:
Risk Management and Healthcare Policy 2021;14 1263–1270 http://doi.org/10.2147/RMHP.S298783
21. Michel, R. Michael J. Z. Implementation of an X-ray Radiation Protective Equipment - Inspection Program. Health Phys. 82 (Supp1ement l): . 2002; S51-53;
22. CRCPD, Quality Control Recommendations for Diagnostic Radiography Volume 3 Radiographic Or Fluoroscopic Machines. Kentucky.Conference of Radiation Control Program Directors, Inc. 2001 available at www.crcpd.org. [Accessed on 22/8/2021].