AN EVALUATION OF THE EVIDENCE OF BURNOUT AMONG ULTRASOUND PRACTITIONERS IN RIVERS STATE
Main Article Content
Abstract
Background: Occupational burnout has become a critical issue among ultrasound practitioners. Inappropriate management of occupational burnout can lead to serious health problems.
Aim: To evaluate the evidence of burnout among ultrasound practitioners in Rivers State.
Materials and methods: A survey of ultrasound practitioners in selected diagnostic imaging facilities in Port Harcourt and its environs was conducted between November, 2018 and March, 2019 to evaluate the evidence of burnout. A descriptive survey design was employed and selection of the facilities was done using systematic sampling technique. 21 diagnostic imaging facilities were used. Ethical clearance was obtained from Management of the facilities. Data were obtained from structured questionnaires administered to 50 ultrasound practitioners in these facilities, who accepted to participate in the study. The questionnaire surveyed basic demographic data, time taken to get to work, experiences, practices, number of night shifts and other factors that predispose burnout. Data analysis was done using SPSS version 20.
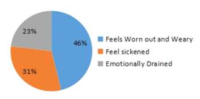
Results: The factors contributing to burnout among ultrasound practitioners are understaffing leading to work overload and excessive overtime work (41%), hostile interactions with patients' relatives (34%), interactions with colleagues (20%), and conflict with Boss/supervisor (5%). Burnout manifests differently among the practitioners as feelings of: being worn-out and weary (46%), being sick (31%), being emotionally drained (23%).
Conclusion: Ultrasound practitioners in Rivers State suffer high level of burnout. Issues of understaffing and interpersonal communication skills should be addressed in order to minimize the incidence of burnout.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
All articles in JRRS are published under the Creative Commons Attribution 4.0 International License (CC BY 4.0). This permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
How to Cite
References
[1] Maslach, C. and Leiter, M. P. The Truth About Burnout: How Organizations Cause Personal Stress and What to Do About It, 1997. San Francisco, CA: Jossey-Bass.
[2] Daugherty, J. M. Burnout: How sonographers and vascular technologist react to chronic stress. Journal of Diagnostic Medical Sonography. 2002; 18(6): 305 -312.
[3] Montero-Marin. J., Prado-Abril, J., Piva Demarzo, M. M., Gascon, S., GarcíaCampayo, J. Coping with Stress and Types of Burnout: Explanatory Power of Different Coping Strategies. PLos ONE. 2014; 9(2): e89090. Available at (https://doi.org/10.1371/journal.pone.0089090).
[4] Carod-Artal, F., Vazquez-Cabrera, C. Burnout Syndrome in an International Setting. Sabine Bahrer-Kohler (Ed.) Burnout for Experts: Prevention in the Context of Living and Working, 2013. Springer Press, New York.
[5] Kim, H. J., Shin, K. H, and Umbreit, W. T. Hotel job burnout: The role of personality characteristics. International Journal of Hospital Management, 2007; 26:421 – 434.
[6] Felton J. S. (1998). Burnout as a clinical entity- its importance in health care workers. Occup. Med., 1998; 48:237 – 50.
[7] Bakker, A., Demerouti. E., Sanz-Vergel, A. Burnout and Work Engagement: The JD–R Approach. Annual Review of Organizational Psychology and Organizational Behavior, 2014; 1(1): 389 – 411. doi:10.1146/annurev-orgpsych031413-091235
[8] Ruotsalainen, J., Verbeek, J., Mariné, A. and Serra, C. Preventing occupational stress in healthcare workers. The Cochrane Database of Systematic Reviews, 2014; 12: CD002892.
[9] Amiri, M., Khosravi, A., Eghtesadi. A., Sadeghi. Z., Abedi, G., Ranjbar, M., et al. Burnout and its Influencing Factors among Primary Health Care Providers in the North East of Iran. PLoS ONE. 2016; 11(12): e0167648.
[10] Simon, M. Nine percent of Nurses across Europe report intent to leave their profession, with burnout among the associated personal and professional factors. Evidence Based Nursing. 2014; 17(2):54 – 55.
[11] Ghorpade, J. Burnout and Personality: Evidence from Academia. Journal of Career Development, 2007; 541 – 559.
[12] Ashil, N. J., and Rod, M. Burnout Processes in Non-Clinical Health Service Encounters. Journal of Business Research, 2011; 64, 1116 – 1127.
[13] Ganster, D. C. and Schaubroeck, R. Work, Stress and Employee Health. Journal of Management, 1991; 17, 235 – 271.
[14] Schuller, N. The factorial validity of the Maslach Burnout Inventory: General Survey across Occupational Groups and Nations. Journal of Occupational and Organisational Psychology, 2000; 73, 53 – 66.
[15] Maslach, C., Schaufeli, W. B. and Leiter, M. P. Job burnout. Ann Rev Psychol., 2001; 52: 3 9 7 – 4 2 2 . doi: 10.1146/annurev.psych.52.1.397.
[16] Schneider, M. E. Occupational burnout among Radiographers, Sonographers and Radiologists in Australia and New Zealand: Findings from a national survey. Journal of Medical Imaging and Radiation Oncology, 2017; 61(3): 304 – 310. doi: 10.1111/1754-9485.12547
[17] Wellis, J. The impact of stress amongst health professionals. Journal of Mental Health, 2011; 20 (2): 111 – 114.
doi:10.3109/09638237.2011.556161.
[18] Rai, G. S. Burnout among Long-Term Care Staff. Administration in Social Work, 2010; 34 (3): 225 – 240.
doi:10.1080/03643107.2010.480887.
[19] Murphy, S. Work Related Musculoskeletal Disorders in Sonography. Society of Diagnostic Medical Sonography white paper
series, 2018. Plano, Texas. Available at (www.sdms.org). Accessed on 11/07/2018.
[20] Steers, R. M. Introduction to Organizational Behaviour, Fourth Edition, 1991. HarperCollins Publishers Inc., New York.
[21] Cooper, C. L. and Marshall, C. S. Healthy mind, healthy organization: A proactive approach to occupational stress. Journal of personnel psychology, 2006; 47(4): 455 – 471.